Apparently Vitamin C is being used in China to “treat” COVID-19? Not so fast.
Just because it’s apparently being used doesn’t mean that it works. Even within the Chinese article itself there is a severe lack of evidence. The article’s ONE citation on Vitamin C is on hemorrhagic hypotension and it is in RATS.
- We also might want to be really skeptical about the traditional Chinese medicine used for COVID-19, especially with the recent fraudulent study covered here by microbiologist, Elisabeth Bik.
The topic of Vitamin C and how it won’t “boost” your immune system against the Coronavirus is also covered here and here.
I find it deeply troubling to see alternative health practitioners trying to promote supplements at this time. Even worse is health food stores and supplement companies are trying to promote products and capitalize on this current pandemic. Taking advantage of people’s fears and posting misleading “immune boosting” product promotions or ways to apparently “protect” oneself from the Coronavirus using supplements is irresponsible, unscientific and should not go unchallenged.
Here is the thing: At the time of writing this, there is ZERO human evidence that any “natural” or “holistic” supplement will prevent or treat COVID-19. There is ZERO evidence that Vitamin C will prevent or treat COVID-19.
With that said, some still think that it will “boost” your immune system. Some still cite evidence for Vitamin C and common colds and inflammation in general. But what does that evidence say and how strong is it for coming to conclusions? Let’s take a look.
What is some of the evidence on Vitamin C?
Cochrane and Harri Hemilä
Something that has been shared around recently is this 2013 Cochrane review on preventing and treating pneumonia with Vitamin C. Not surprisingly, the lead author, Harri Hemilä, also sells a book promoting this Vitamin for infections. All recent positive Vitamin C conclusions seem to be coming from this author, so I am speculative.
What did the authors conclude?
“The current evidence is too weak to advocate prophylactic use of vitamin C to prevent pneumonia in the general population.”
Despite this they also suggest that “therapeutic vitamin C supplementation may be reasonable for pneumonia patients who have low vitamin C plasma levels”. The important thing to keep in mind here is that these patients would have low vitamin levels or they would be deficient. This would justify Vitamin C to treat a Vitamin C deficiency, not pneumonia.
Deficiency is of course a concern, but this can introduce methodological issues when comparing groups. We will come back to this.
Another 2013 Cochrane review on common colds is being shared around. This review does conclude that it might be “worthwhile for common cold patients to test on an individual basis whether therapeutic vitamin C is beneficial for them.” However, “the failure of vitamin C supplementation to reduce the incidence of colds in the general population indicates that routine vitamin C supplementation is not justified, yet vitamin C may be useful for people exposed to brief periods of severe physical exercise. Regular supplementation trials have shown that vitamin C reduces the duration of colds, but this was not replicated in the few therapeutic trials that have been carried out.”
So they recognize that at the time, Vitamin C is not justified for common colds. But what about the studies in physical exercise? The evidence within the review on physical exercise has been cherry-picked by some to try and justify the effect Vitamin C can have, so what is some of the evidence included to support these findings? Some of the studies are almost 30 years old. Now this doesn’t discredit results, however, it does make me skeptical, especially because these findings in exercise have since been challenged.
Importantly, the articles on intense physical exercise have some major limitations and the Cochrane authors say that “..caution should be exercised in generalizing [these findings on physical exercise stress].” Moreover, when trials were restricted to regular doses and not mega, the prophylactic benefit was refuted. Once again though, as we read through the review, these reported benefits are all in extraordinary circumstances and individuals, and most of the benefit is only in the short term. Hence, even if a case was made for Vitamin C and physical exercise, long term there isn’t much of an effect.
A couple examples of the physical activity trials used are here:
- Peters, E. M., Goetzsche, J. M., Grobbelaar, B., & Noakes, T. D. (1993) Vitamin C supplementation reduces the incidence of postrace symptoms of upper-respiratory-tract infection in ultramarathon runners.
Some important points when looking are that they had an inadequate control and all of the intake and symptom data were self reported. Exercise also reduces Vitamin C concentrations, which makes this trial similar to others with inadequate controls.
- Constantini, N. W., Dubnov-Raz, G., Eyal, B.-B., Berry, E. M., Cohen, A. H., & Hemilä, H. (2010). The effect of vitamin C on upper respiratory infections in adolescent swimmers: a randomized trial.
This study looking at adolescent swimmers found that the benefits on upper respiratory infection duration were only significant in males, a novel finding. Otherwise, there was no effect of Vitamin C on the incidence of upper respiratory infections. Their words: “We did not find any effect of vitamin C on the incidence of URI”.
This physical exercise high dose Vitamin C and E study looking at repeated Taekwondo competitions also found to lower the systemic inflammatory response, however, this was only in the short term. Moreover, this study that mimicked Olympic or international level Taekwondo competition does not translate to the general public. This study echos the same result as the previous ones: short term benefit in extraordinary individuals.

This effect for exercised induced inflammation has been challenged though: “These findings indicate that pre-exercise supplementation of ascorbic acid does not alter oxidative stress markers in the plasma and erythrocytes of young adults engaged in a supervised exercise program.” Once again, there does not seem to be significant long term benefits when looking at these studies in exercise.
Plus, an increase in immunity, or really what is actually maintenance of immunity or coming back to baseline, could be attributed to multiple factors after physical exercise. The improvement using Vitamin C in ultra marathon runners could just be because they are no longer in such a high stress environment anymore. A good review on the topic and general recommendations can be found here.
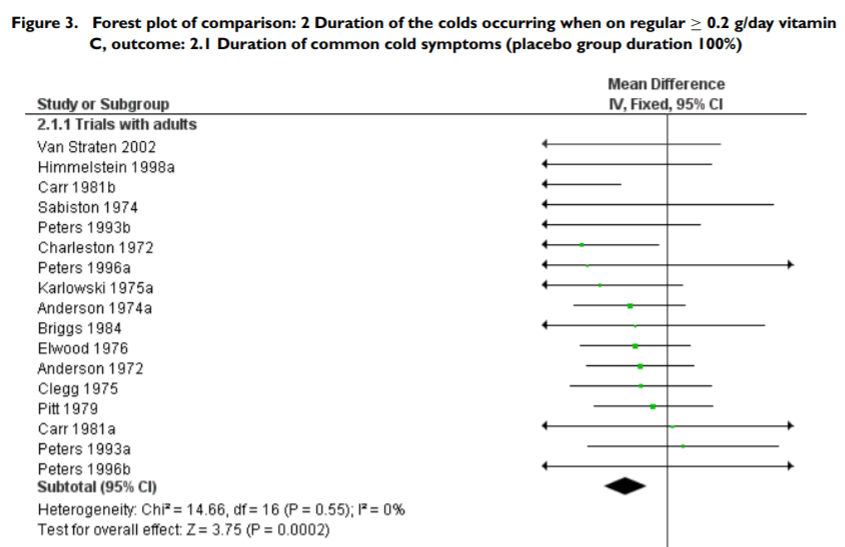
Looking a the forest plots in this Cochrane review, I am confused. I think this might go to show that just because the forest plot favors an intervention or not, doesn’t mean that the evidence used is strong. Essentially, I am not very confident in these forest plots.
If we look at Figure 3 (below) for example, and let’s say we will focus on the study: Carr 1981b.
By looking at the forest plot this study helped shift the effect to favor Vitamin C for cold duration in adults. However, the common cold data is self-reported and they even conclude that “there was no effect of vitamin C in preventing colds.” The placebo was even said to be effective, but keep in mind that these were subjective feelings.
This does NOT give any evidence that placebo effect should be used to treat or prevent colds. Plus people always try to use this as a justification for Homeopathy and we know that Homeopathy is useless. In fact, in a study looking at the effects of placebo and the common cold, “illnesses were substantively shorter and less severe” in those experiencing the placebo effect. HOWEVER, there was no statistically significantly change in interleukin 8 concentration and neutrophil cell count between groups and “results of this trial do not support a powerful placebo effect in the common cold.”
They also include the trial by Anderson from 1972, which helps shift the effect on incidence of colds to favor Vitamin C in the general population (Figure 2, not shown here), however, it’s not that promising. “It was found that in terms of the average number of colds and days of sickness per subject the vitamin group experienced less illness than the placebo group, but the differences were smaller than have been claimed and were statistically not significant. However, there was a statistically significant difference between the two groups in the number of subjects who remained free of illness throughout the study period.” The authors have a hard time coming to conclusions about this though since at the time, more research was required.
Another important point is that most of the studies, since quite a few are from the 1970s, try to build off of Linus Pauling’s work. Many are in support of Pauling in these studies, however, in 2020 much has changed. The history of Pauling’s claim to fame became anything but positive is detailed here by Paul Offit. Another problem here is that even in the 1970s, these findings were criticized: “Benefits shown have been modest, and positive findings have not been reproducible. Reported benefits probably are due to statistical artifact, minor vitamin-induced physiologic changes, the placebo effect, or a combination of these.”
Another disappointing review by Harri Hemilä
Unfortunately, this review article places most of the weight on only TWO studies. They once again are dated and when you look at them, they aren’t strong evidence. Some points about them are included below.
- Changes in Leucocyte Ascorbic Acid during the Common Cold: Small study. Confounded by low leucocyte ascorbic acid levels, guess what though, “the changes in L.A.A. were similar to that of the subjects not ingesting ascorbic acid.” This does not provide evidence of efficacy of Vitamin C in common colds.
- Winter illness and large doses of Vitamin C: “None of the groups receiving vitamin C showed a difference in sickness experience that was statistically significant..” As said by the authors, most differences were statistically non significant and should be interpreted with caution. The study contained other limitations too.
What did a previous review in 2006 conclude?
- “The lack of effect of prophylactic vitamin C supplementation on the incidence of common cold in normal populations throws doubt on the utility of this wide practice.”
Randomized Controlled Trials?
The second Cochrane review talked about above, the 2013 one on common colds, calls for more RCTs. However, they do exist.
This one is even included in the review: “Preventive treatment of healthy children with vitamin C in large doses this had no definitely proved effect against colds.”
Here’s something that is troubling me though. I am curious if there is selection bias with regards to the studies included for the review. Now, they do mention why in their exclusion criteria, however, they also recommend looking at the studies that were excluded.
Meta analysis of Randomized Controlled Trials (RCTs)
This Meta analysis of RCTs does conclude that taking “extra doses of vitamin C could benefit some patients who contract the common cold”. However, once again, the data is not promising. When looking at the Duration of the Main Symptoms, pretty much all of them are not significant for Vitamin C when compared to placebo.
Out of the seven common symptoms (nasal congestion or runny nose, sore throat, fever, aching limbs and muscles, chest pain, chills, and mental depression) looked at, only three just barely favored Vitamin C.



Even with these trials though, their findings might not be clinical meaningful in the slightest. Chills were reduced by only 8 hours and fever was reduced by half a day.
Another important point is that the authors found high publication bias.

The authors also mention in their Limitations that, “in some cases the data has to be calculated and transformed rather than being available directly.” In my opinion, this further weakens the positive conclusions in this Meta analysis.
Review of RCTs for Vitamin C and Neutrophil Function
Another important consideration about Randomized Controlled Trials looking at immune and Neutrophil function is that the majority are heterogeneous and lack proper controls:
- “Unlike drug trials, evidence indicates that RCTs of vitamin C supplementation will be more likely to have a positive effect in participants who are suboptimal or deficient in the vitamin at baseline. Therefore, future RCTs should incorporate prescreening of potential participants for low vitamin C status or utilize cohorts known to have low vitamin status, such as hospitalized patients.” Once again, we come back to methodological issues when comparing groups. This goes for the trials in physical activity as well as groups with suspected vitamin deficiency.
Plus, this review found that, “Overall, nine of the 16 RCTs included in this review reported no effect of supplementation with vitamin C alone, or in combination with other micronutrients or antioxidants, on various neutrophil functions”
To repeat what was said above, the studies that did find positive results were in hospitalized patients or outpatients or athletes. “None of the other studies carried out with healthy volunteers showed any effects of additional supplementation.”
What about the effects on immune cells? “Eight of 10 RCTs showed no effect of supplementation on neutrophil phagocytosis and/or oxidative burst activity “
“It should also be noted that neutrophils saturate at lower vitamin C levels than plasma [50]. Therefore, it is unlikely that supplementing healthy volunteers or athletes with additional vitamin C over and above their normal baseline levels would have an effect on neutrophil function [51].”
Vitamin C Trials on Sepsis and Inflammation
When it comes to assessing the effects of Vitamin C on inflammation, etc., we can turn to randomized clinical trials looking at “inflammation and vascular injury associated with sepsis and acute respiratory distress syndrome”. In this case these two trials looked at Intravenous (IV) Vitamin C, which also a common Naturopathic treatment for sepsis due to it’s assumed anti-inflammatory benefits. What does the actual rigorous evidence say?
The 2019 CITRIS-ALI Trial:
- “In this preliminary study of patients with sepsis and ARDS, a 96-hour infusion of vitamin C compared with placebo did not significantly improve organ dysfunction scores or alter markers of inflammation and vascular injury.”
The 2020 VITAMINS Trial:
- “In patients with septic shock, treatment with intravenous vitamin C, hydrocortisone, and thiamine, compared with intravenous hydrocortisone alone, did not significantly improve the duration of time alive and free of vasopressor administration over 7 days. The finding suggests that treatment with intravenous vitamin C, hydrocortisone, and thiamine does not lead to a more rapid resolution of septic shock compared with intravenous hydrocortisone alone.”
What is a clinical feature of COVID-19? Increased C-reactive protein (a marker of inflammation), as reported here and here.
What doesn’t Vitamin C improve compared to placebo? C-reactive protein.
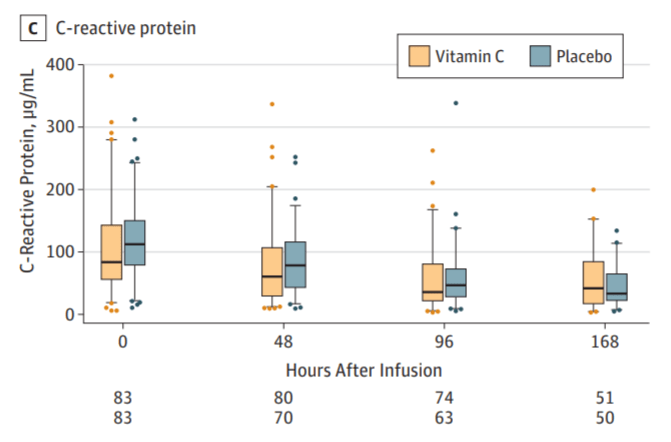
In this CITRIS-ALI trial, there was a lower mortality rate in the Vitamin C group. However, “differences in baseline characteristics of this necessarily heterogeneous population may have influenced mortality.” This was explained further here. Another consideration is that while different in their interventions, the VITAMINS trial did not show a significant difference in mortality. Another 2019 trial also found no improvement in survival.
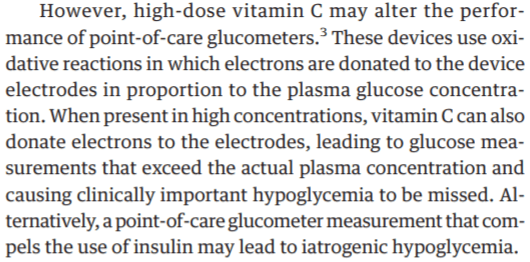
- There is also some concern about high-dose vitamin C altering the performance of point-of-care glucometers, “leading to glucose measurements that exceed the actual plasma concentration and causing clinically important hypoglycemia to be missed.”
The lack of effect for antioxidant supplements in general for inflammation has been echoed in the literature.
- In 2017: Overweight/obese female adults were either given a chewable tablet (included vitamin C, wild bilberry fruit extract, green tea leaf extract, quercetin, caffeine, and omega 3 fatty acids) or placebo. After 4 weeks, “Groups did not differ in markers of inflammation (IL-6, MCP-1, CRP) or oxidative stress (oxLDL, FRAP).”
- In 2018: Generally healthy adults were told to either 1) consume their usual diet combined with antioxidant supplements 2) or a placebo supplement pill, 3) or their usual diet combined with increased antioxidant-rich food intake plus a placebo pill. “There were no significant changes in any of the three inflammatory markers investigated, regardless of the source of antioxidants from diet or supplements, despite evidence from blood sampling and dietary records that overall antioxidant intake was substantially increased.” (Refer to the Figure 2 Box Plot.) This study further underscores the fact that if you are already in good health, antioxidant supplementation or consumption of antioxidant-rich foods [will most likely] not lower concentrations of the specific markers of inflammation…”
Cytokine Storm and IL-6
One noticeable feature of the “cytokine storm”, that is characteristic of mild to severe COVID-19, is an increase in IL-6.
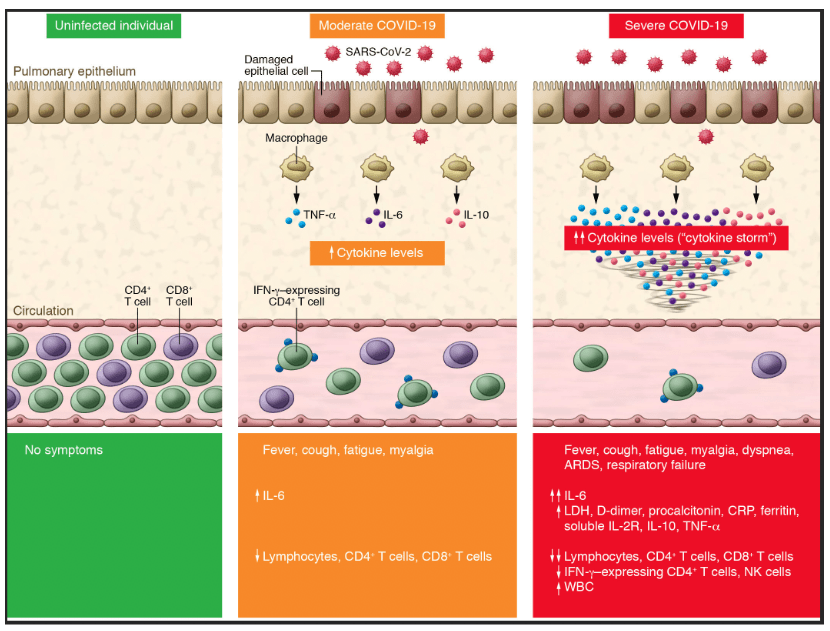
As said above, the addition of a chewable antioxidant tablet did not improve markers of inflammation, including IL-6. The same result was found with antioxidant rich diets and supplements. Based on findings from Lu Q and colleagues, it does not seem like continuous oral treatment with ascorbic acid significantly impacts IL-6, as well as IL-1ra and hs-CRP levels, compared to placebo in Type 2 Diabetics. However, Ellulu et al. found the opposite. Given that the study by Lu Q et al. had no significant decreases in markers like HbA1C or plasma glucose, but Ellulu et al. did, it is possible that the improvements in these markers influence the improvements in IL-6. In chronic smokers, only the combination of Vitamin C and 800 IU Vitamin E reduced IL-6. Vitamin C with 400 UI of Vitamin E and Vitamin C alone did not change the levels of IL-6. In terms of prevention, Vitamin C supplementation did not influence the exercise induced increased in IL-6 and IL-10.
Conclusion
We can confidently say that even though China might be using Vitamin C, this doesn’t mean that this decision is scientifically sound. At the time of writing this, there is ZERO human evidence that any “natural” or “holistic” supplement will prevent or treat COVID-19. There is ZERO evidence that Vitamin C will prevent or treat COVID-19. The evidence that Vitamin C will “boost” your immune system, prevent and treat the common cold or significantly improve inflammation is extremely weak and unlikely. Given the overall scientific evidence, promoting supplements, such as Vitamin C, for COVID-19 is incredibly irresponsible and misleading.
Some additional links:
- Boosting immunity for COVID-19? Only when we get a coronavirus vaccine.
- Coronavirus prevention – quacks are using the anti-vaccine woo cookbook
- Immune system boosting myths
- Flu treatments and supplements – do they work? No, get the vaccine
- Alternative Medicine Exploits Coronavirus Fears
- Coronavirus quacks get smacked down by the FDA
- Coronavirus homeopathic potions – here comes the quackery and woo
- Misinformation, alternative medicine and the coronavirus
- FTC & FDA: Warnings sent to sellers of scam Coronavirus treatments
- How Linus Pauling duped America into believing vitamin C cures colds
- Boost Your Immune System?
- More Boosting the Immune System
- Immune Boost Bunk
- Elderberry Elixir for the Common Cold
- Updates and edits will be added as necessary.
